Bacterial Vaginosis - Causes, symptoms and treatment
- Marketing cheryl
- Jan 12, 2023
- 3 min read
Updated: Jul 1, 2024

Have you ever heard of the term “urogenital infection”? As the name suggests, urogenital infections refer to infections concerned with our genitalia and urinary tract. These infections affect around 1 billion people in the world annually¹ and are more common in women than in men.² One of the most common urogenital infections that women face is known as Bacterial Vaginosis (BV), a type of bacterial infection of the vagina.
BV is a common urogenital infection, resulting from an overgrowth of bad bacteria in our vaginal flora (the various bacteria living in our vagina). In healthy women, the vaginal flora is dominated by a species of good bacteria called Lactobacillus, but women with BV have a vaginal flora that is made up of a more diverse and harmful combination of bad bacteria, with a decreased amount of beneficial Lactobacillus.³
Why is Lactobacillus important?
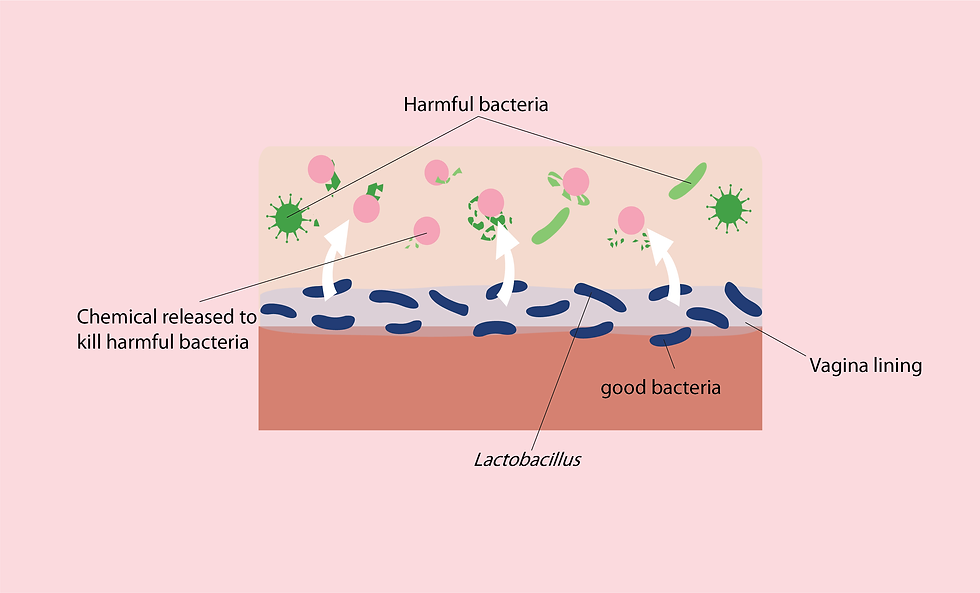
There is a reason why Lactobacillus bacteria is the dominant bacteria present in our female vaginal flora. This species of good bacteria is what keeps our vagina healthy, as Lactobacillus produce chemicals that kill yeast and harmful bacteria, thus preventing infections.⁴ On top of that, Lactobacillus also prevents such harmful bacteria from adhering to our vaginal walls, rendering these harmful bacteria to be unable to infect our vagina.
However, the bacteria composition of our vagina may change due to various factors such as:
Stress
Hormonal imbalance
Having a new sexual partner
Having multiple sexual partners
Regular douching⁵
These changes may lead to having more bad bacteria in our vaginal flora. Additionally, such habits also make our vaginal environment less acidic, which in turn makes it more conducive for bad bacteria to thrive in, potentially leading to BV.
When experiencing BV, our vaginal discharge usually becomes thinner with a white or greyish colour. We also experience increased production of a substance called amine in our bodies. These amines carry a fishy odour and as you might have guessed, comes out with our vaginal discharge to produce an unpleasant fishy odour.
I’ve had these urogenital symptoms and have never gone to a doctor! Should I be worried?
If your BV symptoms such as having increased discharge with fishy odour persist and you start experiencing itch or irritation, you may want to consider visiting a doctor for treatment. Depending on the severity of the infection, doctors may prescribe antibiotics for the treatment. However, antibiotics alone can only temporarily cure the infection, they do not prevent the relapse of BV.
So how do we reduce the recurrence of BV?
We can prevent BV from recurring by doing our best to maintain the healthy balance of our vaginal flora. This includes changing certain habits such as douching, or incorporating probiotic supplementation into our lifestyle.
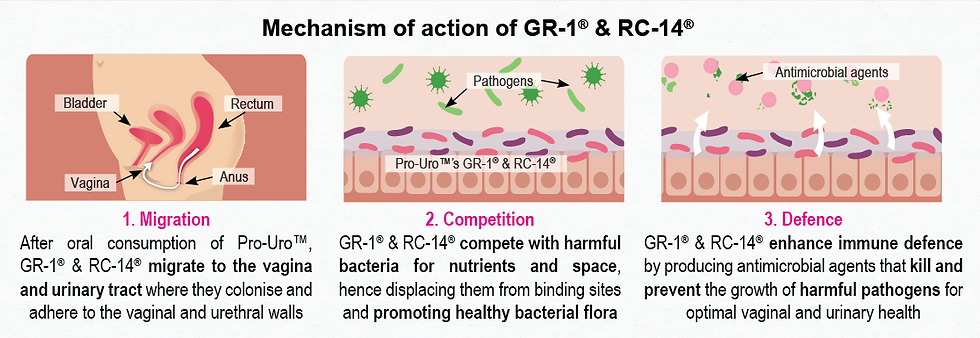
Clinical research has found that probiotics such as GR-1® & RC-14® in Pro-Uro® can populate our urogenital tract with beneficial Lactobacillus. These Lactobacillus can enhance our vaginal health and protect us against urogenital infections.
GR-1® and RC-14® probiotics are found in Pro-Uro®. Both of these probiotic strains have shown significant efficacy in managing BV.⁶
In a clinical study involving 125 women between the age of 18 to 44 years old, it was found that GR-1® & RC-14® were able to increase the cure rate of BV in these patients. GR-1® and RC-14® probiotic strains belong to the Lactobacillus species and work to rebalance our vaginal flora to maintain optimal vaginal health and prevent urogenital infections. Thus, consuming Pro-Uro® probiotics can help prevent BV from recurring.
With our clinically proven Pro-Uro®, you’ll be able to reduce BV occurrences more effectively. Take charge of your urogenital health today with Pro-Uro®!
References
Reid, G., Bruce, A.W., Fraser, N., Heinemann, C., Owen, J. and Henning, B. (2001). Oral probiotics can resolve urogenital infections. FEMS Immunology & Medical Microbiology, [online] 30(1), pp.49–52.
Harrington, R.D. and Hooton, T.M. (2000). Urinary tract infection risk factors and gender. The journal of gender-specific medicine: JGSM: the official journal of the Partnership for Women’s Health at Columbia, [online] 3(8), pp.27–34.
Homayouni, A., Bastani, P., Ziyadi, S., Mohammad-Alizadeh-Charandabi, S., Ghalibaf, M., Mortazavian, A.M. and Mehrabany, E.V. (2014). Effects of Probiotics on the Recurrence of Bacterial Vaginosis. Journal of Lower Genital Tract Disease, 18(1), pp.79–86.
www.cdc.gov. (2022). STD Facts - Bacterial Vaginosis. [online] Available at: https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm#:~:text=BV%20is%20a%20result%20of.
Sobel, J.D. (2017). 53 - Vaginitis, Vulvitis, Cervicitis and Cutaneous Vulval Lesions. [online] ScienceDirect. Available at: https://www.sciencedirect.com/science/article/pii/B9780702062858000538
Han, Y. and Ren, Q., 2021. Does probiotics work for bacterial vaginosis and vulvovaginal candidiasis. Current Opinion in Pharmacology, 61, pp.83-90.
Disclaimer: The article content is intended for informational or educational purposes only, and does not substitute professional medical advice or consultations with healthcare professionals. The disclaimer also provides that no warranties are given in relation to the medical information supplied in the article, and that no liability will accrue to Miraco Nutripharm Pte Ltd or any affiliated authors in the event that a user suffers loss as a result of reliance upon the information.




I want to thank Dr. Riaria for helping me with his herbal medicine to cure my herpes virus completely without any side effects, i really suffered from this virus for the past 3 years, Right now I'm herpes negative after using the herbal medicine sent to me by Dr. Riaria. I gave all thanks to God for leading me to Dr. Riaria who was able to cure me completely from herpes virus, you are the best traditional herbal doctor in the world, God bless you sir. Contact him via email: drriaria@gmail.com or WhatsApp him on +2347010627760.
You can check on his website for more Info:
https://drriaria.wixsite.com/website
I recommend you to get your herbal medicine through Herbal Miracle Medicine . He cured me from my herpes outbreak and now I am free . All thanks for your care and giving me my life back . If you are suffering from any illness you can get your medication from Doc Moses Buba on his .
email him on ( buba.herbalmiraclemedicine@gmail.com )
Facebook page: https://www.facebook.com/profile.php?id=61559577240930
website:https://bubaherbalmiraclem.wixsite.com/website